Supporting Your Sexual
(& Reproductive) Health
Whether you're sexually active or not, there are things you can do to support your sexual health.

Sexual Activity and You
When it comes to sexual activity, there’s a wide range of experiences. Whether you haven’t been sexually active at all, have some experience, or have had many experiences, you’re in good company. There's lots of people having sex and lots of people not.
People might practice abstinence for a variety of reasons-personal beliefs and values, culture or religion, or simply not being interested. And people have sex for lots of reasons-pleasure, connection, expressing love or affection, and personal exploration. All of these are valid choice and important to know about yourself.
While abstinence is the only 100% effective way to prevent pregnancy and sexually transmitted infections (STIs), there are a lot of other options to reduce risks if you're currently sexually active or decide to be sexually active later on. Knowing these options can help you make the best decisions for yourself.
Supporting Your Sexual Health Wherever You Are
There are lots of things everyone can do to support their sexual health to care for themselves and current/future partner(s). Healthcare, education, and safer sex practices can help anyone now or in the future.
Healthcare Can Support Your Sexual Health
Sexual Health Checkups & STI Screenings
These are a great opportunity to check in on your overall well-being, get screened for STIs, explore birth control options, and ask any questions you might have. These visits aren’t just for people who are sexually active—they’re a smart way to stay informed, catch any issues early, and take charge of your health.
HPV Vaccination
The Human Papillomavirus (HPV) Vaccine is highly effective in preventing genital warts, oral cancer, cervical cancer, and many other types of cancer caused by HPV.
This vaccination is recommended for all genders with routine vaccination starting at age 11-12 through the age of 26. If you're over 26, check with your healthcare provider, as it's a case by-case-basis.
PrEP, PEP, and HIV
Pre-Exposure Prophylaxis (PrEP) and Post Exposure Prophylaxis (PEP) are antiretroviral drugs that can help lower the risk of acquiring HIV. Talk with your healthcare provider about your options.
PrEP is a daily pill that can help lower the risk of acquiring HIV.
PEP involves taking medication AFTER a high-risk exposure to stop HIV seroconversion. PEP must be started within 72 hours of possible exposure.
Safer Sex Is Part of Sexual Health
You deserve to feel supported and in control of your sexual health. If you're sexually active or planning to be, learning about safer sex practices—like birth control, STI prevention, and protection options—helps protect both you and your partner(s). Knowing your options ahead of time is one of the best ways to make decisions you feel good about.
Barrier Methods Reduce Risk
Barrier methods are an easy and effective way to reduce the risk of sexually transmitted infections (STIs). External and internal condoms also reduce the risk of pregnancy by creating a physical barrier to prevent sperm from entering the body. They're also relatively easy to get - whether free of cost at local health centers or for purchase in stores or online.
Key things to keep in mind:
- use a protective a barrier each time for oral, vaginal, or anal sex
- they are only as effective as their user
- use a new one each time for each act
- do not double up Use a new one every time
3 Main Types of Barrier Methods

External Condoms
Worn on the penis or sex toys during oral, vaginal, or anal sex, external condoms are the only birth control method that also protects against STIs. They’re usually made of latex, but non-latex and flavored options are available. When used correctly every time you have sex, they are up to 98% effective at preventing pregnancy. For added protection, they can be used with other methods like the pill, IUD, or PrEP.
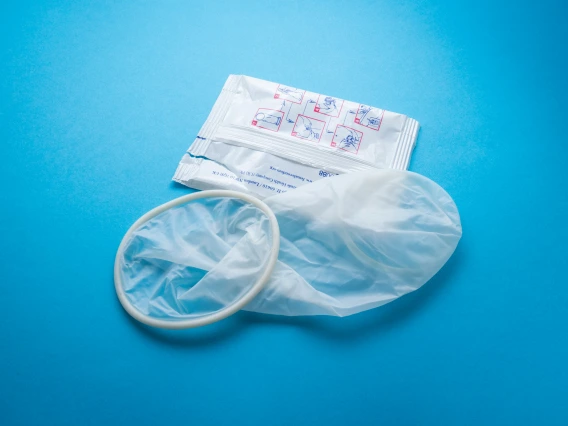
Internal Condoms
Sometimes called "female condoms", are worn inside the vagina or anus. They’re made of a soft, thin material that lines the inside of the vagina for protection.
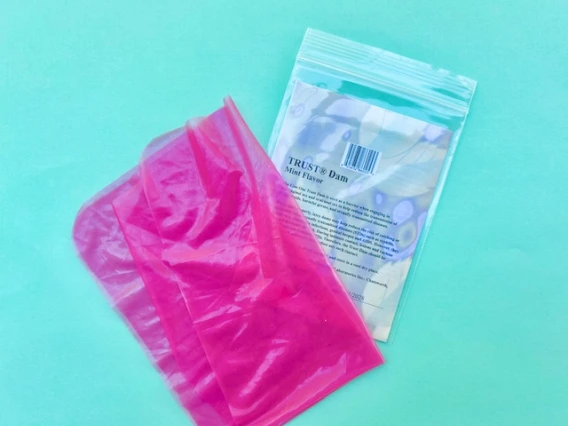
Latex Dams
Also known as dental dams, these are thin sheets of latex (or other materials) that act as a barrier during oral sex to reduce the risk of STI transmission. They come in a variety of flavors and colors.
Sexually Transmitted Infections (STIs)
Sexually transmitted infections (STIs) are spread through sexual contact—including vaginal, oral, and anal sex. They’re more common than you might think—millions of new cases are reported each year in the U.S.
The good news? All STIs are preventable and treatable—and most are even curable. Being informed, using protection, and getting tested regularly are simple ways to reduce your risk of contracting or spreading an STI.
Signs & Symptoms
Commonly, STIs have no symptoms or very mild symptoms, which is why it's possible to have an STI and not know it.
Other symptoms of an STI can include: itching or irritation, burning during urination, sores, bumps, blisters, pain during sex or urination, unusual discharge from the vagina, penis or anus, and pain in the lower abdomen.
If you notice anything unusual, even if you don't have symptoms, get checked out by a medical provider.
STI Testing
STIs can be caused by viruses, bacteria, fungi, or parasites—which means there’s no one-size-fits-all test. Some require a blood or urine sample, others a swab or physical exam. That’s why it’s important to talk openly with your healthcare provider about your sexual activity—they can help you figure out which tests you need. If you're having sex, getting tested regularly is a key part of staying healthy.

Birth Control Options
Birth control reduces the chance of pregnancy and there are many types of birth control—both hormonal and non-hormonal—so you have options. From pills, patches, and IUDs to condoms and fertility awareness methods, the best birth control is the one that works for you and your lifestyle.
Explore birth control methods in-depth
Non-Hormonal Birth Control
Non-hormonal birth control methods are a great choice if you prefer to avoid hormones, have certain health conditions, or ???. They include internal and external condoms, withdrawal, fertility awareness methods, diaphragms, the copper IUD, and cervical caps. Condoms are the only one of these methods that protects against STIs.
Hormonal Birth Control
Hormonal birth control works by preventing ovulation (the release of an egg) and thickening the cervical mucus, which makes it harder for sperm to reach an egg. Most hormonal methods use a combination of progestin and estrogen.
Hormonal birth control comes in different forms—like the pill, patch, ring, shot, and IUD—and works for varying lengths of time. Just remember: hormonal methods do not protect against STIs, so using condoms, as well, is a smart way to stay safer.
Long Acting Reversible Contraceptives (LARCS)
With up to 99% effectiveness, LARCS have the highest effectiveness rate of all birth control options. LARCS include IUDs (hormonal and non-hormonal options) and the arm implant. These options require insertion and removal by a medical provider.

Choosing A Form of Birth Control
With all the options available, there are pros and cons to each one depending on what you're looking for. You can compare methods side by side to see their effectiveness, side effects, cost, effort, health benefits, and more.
Communicate with Your Partner(s) In Support of Your Sexual Health
Communication might not be the first thing that comes to mind when it comes to sexual health, but it can help make sex more enjoyable, help you feel more empowered, and reduce risk. Everything on this page is a great talking point.
Here are some examples of what you might want to talk about:
Consent Is Part of Communication

Pointers for Talking About Sex
There's lots of reasons people do or don't have sex. There are also a lot of feelings that can come up about sex. When you talk about sex, it's helpful to keep these things in mind to make sure everyone's feeling safe, heard, and connected.
Do
- talk how you would want to be talked to
- know and communicate your boundaries
- provide a context for the conversation
- plan to have the conversation so both you and your partner(s) can be prepared
- use "I" statements and focus on the people in the relationship
- have a collaborative and solution-focused attitude
- share how you feel
Avoid
- pressure
- blaming
- judgment
- catching someone off-guard
- comparing to past partners
- making someone or something a problem
